The Center for Reproductive Rights is a global human rights organization of lawyers and advocates who ensure reproductive rights are protected in law as fundamental human rights for the dignity, equality, health, and well-being of every person.
In the U.S., one in four women will end a pregnancy in her lifetime—yet because of a decades-long effort by anti-abortion lawmakers, 90% of counties are without a single abortion provider. And although most U.S. maternal deaths are preventable, the country has the highest maternal mortality ratio among wealthy nations. In addition, contraception and assisted reproduction services are often unaffordable and out of reach for many.
Through strategic litigation and legal policy and advocacy, and by holding governments accountable, the Center’s U.S. Program—with offices in New York and Washington, DC—works to strengthen legal guarantees to ensure that reproductive rights and health services are available across the country. The Center is especially focused on reducing disparities in accessing care, since Black, Indigenous and people of color, and those living in rural communities and with lower incomes, are disproportionally harmed when health care is inaccessible.
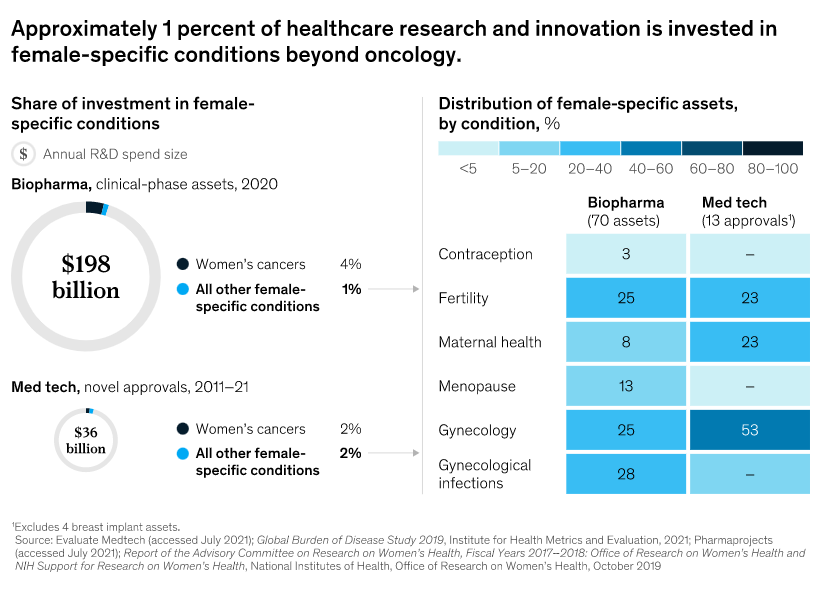
There are significant opportunities for healthcare providers to consider reallocating resources to female conditions, including the following:
Maternal health: More than 800 women die globally every day from pregnancy- and childbirth-related causes, including hemorrhages and infections.16 The tragedies are not confined to emerging economies; even before the outbreak of COVID-19, the maternal mortality rate in the United States doubled between 2002 and 2018, with Black women disproportionately affected.17
Endometriosis: One in ten women of reproductive age is estimated to have endometriosis (growth of endometrial tissue outside of the uterus), which can cause debilitating pelvic pain and infertility. The underlying pathophysiology is poorly understood, diagnosis takes ten years on average, and there is currently no cure.18
Menopause: Women spend more than a third of their lives in peri- or post-menopause, and trends indicate that 1.2 billion women globally will be in these life stages by 2030.19 The vast majority of women find that menopausal symptoms such as hot flashes, night sweats, and sleep disturbances interfere with their lives, yet only a quarter obtain treatment.20 The economic impact is significant, with one study estimating nearly $1,400 in health costs and $770 in lost productivity per person per year for untreated hot flashes alone.21
There is great potential to begin addressing these conditions in new ways. A suite of scientific advances can now be harnessed in women’s health. Recent advances in genomics, tissue engineering, and cell and gene therapy are ushering in a new wave of healthcare innovations that can be applied to underserved female-specific conditions. For example, researchers are studying transcriptomics (the study of all RNA molecules in a cell) for treating otherwise elusive conditions such as preeclampsia or preterm birth. Others are now using tissue engineering to create uterine organoids in order to push the knowledge frontier on endometriosis. The potential is vast to redefine a host of conditions, including endometriosis, preeclampsia, and unexplained infertility, and to achieve advances to the degree that researchers are already achieving with oncology and immunology. Investors, researchers, and companies alike have an opportunity to participate in this rising wave of innovation and to deliver a new era in women’s health.
The maternal death ratio for Black women (37.1 per 100,000 pregnancies) is 2.5 times the ratio for white women (14.7) and three times the ratio for Hispanic women (11.8).
Causes of death vary widely, with death from hemorrhage most likely during pregnancy and at the time of birth and deaths from heart conditions and mental health–related conditions (including substance use and suicide) most common in the postpartum period.
Compared with women with private health insurance, women with Medicaid coverage were more likely to report:
No postpartum visit
Returning to work within two months of birth
Less postpartum emotional and practical support at home
Not having decision autonomy during labor and delivery
Being treated unfairly and with disrespect by providers because of their insurance status
Not exclusively breastfeeding at one week and six months.