HEALTHCARE
Protect women’s rights to make their own reproductive-health decisions by keeping abortion accessible and legal.
• Increase access to mental health and substance-dependency treatment and decriminalize mental health-related crimes.
• Require immunizations for all school students, except where medically contraindicated.
• Increase funding for rural hospitals, including support for migrant and indigent care.
• Permit assistance in dying under carefully considered and clearly specified conditions.
a. Increase access to insurance that enables patient autonomy by favoring home and community-based services over institutional care.
b. Increase access to state-regulated assisted-living facilities, at-home or residential eldercare, palliative care and hospice.
c. Guarantee that any assistance-in-dying law’s “triggers” reflect individual end-of-life prognoses.
d. Ensure the state has capacity to enforce safeguards and any physician who is negligent in applying ordinary standards of care is subject to legal liability.
The All of Us Research Program is inviting one million people across the U.S. to help build one of the most diverse health databases in history. We welcome participants from all backgrounds. Researchers will use the data to learn how our biology, lifestyle, and environment affect health. This may one day help them find ways to treat and prevent disease.
The time for single-payer Medicare for All is now.
Our nation spends more than twice as much per person on healthcare as other countries, and yet tens of millions of Americans still can’t get the care they need. At the same time, corporations in the insurance, pharmaceutical, and hospital industries continue to make billions of dollars in profits while costs increase unchecked. Our profit-driven health care system makes a few incredibly wealthy while leaving so many American families, especially in communities of color, to suffer and die simply because they can't afford the care they need in the wealthiest nation in the history of the world. In 1966, Martin Luther King Jr. said, "Of all the forms of inequality, injustice in healthcare is the most shocking and inhumane." 54 years later, we must finally join the rest of the industrialized world and guarantee healthcare to all of our people as a right.
The Predatory Debt Collection Protection Act
In Arizona, interest rates of medical debt can increase by as much as 10% per year, every year. Families can lose their homes, cars, or have their wages garnished by predatory debt collectors – even if they’ve done everything right.
The Predatory Debt Collection Protection Act fixes these problems by:
Protecting more assets from being sold to pay off debt collectors.
Ensuring hard-working Arizonans keep more of their bank accounts and wages.
Limiting the outrageous interest rates that trap families in an unending cycle of medical debt.
Arizona ranks as the 10th worst state in the country for death rates of mothers in the first year after they give birth.
Medicaid coverage for new mothers should expand from 60 days to 12 months. This change would benefit many families in the state's low-income and marginalized communities, who have little or no access to affordable health care. Black and Indigenous women are two to three times more likely to die than white women within the first year after giving birth
The American Rescue Plan Act, signed into law on March 11, 2021, makes available an additional pathway that allows states to extend Medicaid coverage for pregnant people from 60 days to one year postpartum. This pathway—known as a state plan amendment (SPA)
"We have challenges in Arizona with postpartum deaths"
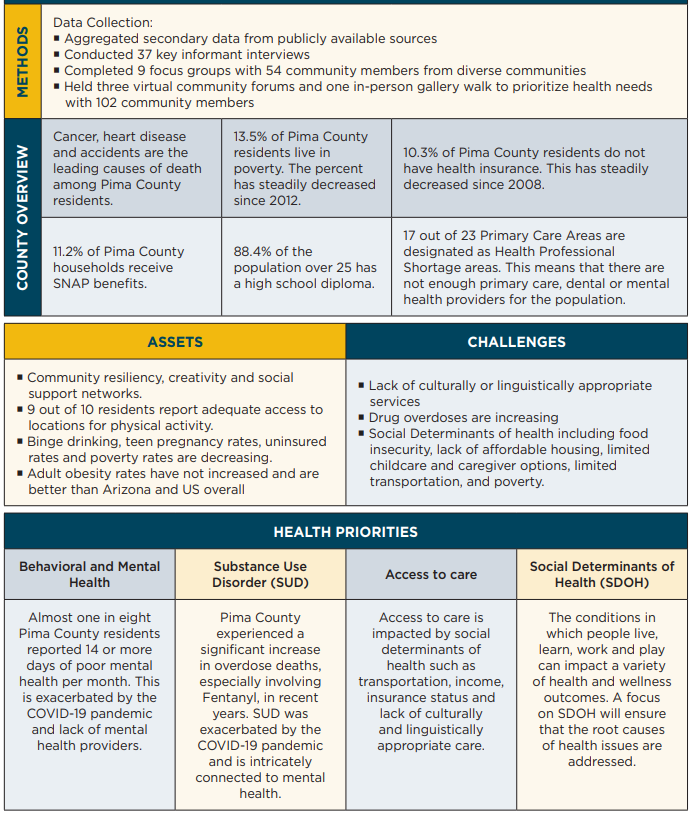
Social determinants of health (SDOH) have a major impact on people’s health, well-being, and quality of life. Examples of SDOH include:
Safe housing, transportation, and neighborhoods
Racism, discrimination, and violence
Education, job opportunities, and income
Access to nutritious foods and physical activity opportunities
Polluted air and water
Language and literacy skills
Master Plan for Aging (MPA) is a cross-sector, state-led strategic planning process that results in a roadmap that can help states transform the infrastructure and coordination of services for their rapidly aging population. An MPA is a living document that provides a clear framework to address the needs of older adults, people with disabilities, and caregivers, for 10 years or more. An MPA:
Enables governors and/or legislative leaders to communicate a clear vision and priorities for their state;
Guides state and local programs, public and private initiatives, policies, and funding to support aging with dignity;
Reflects extensive input from the community, including people of all ages and abilities, actively considering the needs of populations facing racial and ethnic disparities; and
Is evidence-based and uses data and benchmarks for accountability.
Health care workers (HCW) and first responders (FR) working during a pandemic experience a variety of acute and sustained stressors, including fear for their own safety and that of their colleagues and family, exposure to death and suffering, separations from family, and prolonged periods of exhaustion and vigilance.
Health care workers were suffering burnout and more before the pandemic. And there are worrisome trends among educators and other worker groups, too. Indeed, the U.S. in general is experiencing rising anxiety and depression. The U.S. needs sweeping investment in psychiatric disorder prevention and treatment. A critical step in that pursuit is ensuring the well-being of the health care workforce through structural and cultural changes:
Better access to evidence-based psychiatric treatment, including paid sick leave and explicit supervisor encouragement. Insurance should facilitate preference- and need-matched care. Outreach to workers who may be experiencing particularly acute distress, such as EMS personnel, is needed.
More protection and support for workers by health care leaders, from addressing staffing shortages to prioritizing transparent, honest, bidirectional communication that centers frontline workers’ concerns, is needed, along with realistic leave and staffing policies, such as for parents with quarantined children. Factors like systemic racism that compound stress for health care workers of color must be addressed.
Unequivocal support for science-backed measures by political leaders, including vaccines and masking.
Assessing Risk When Everyone's Afraid:
The Challenge of Seeing Health Care Workers as People When Our Need for Them Is So Great
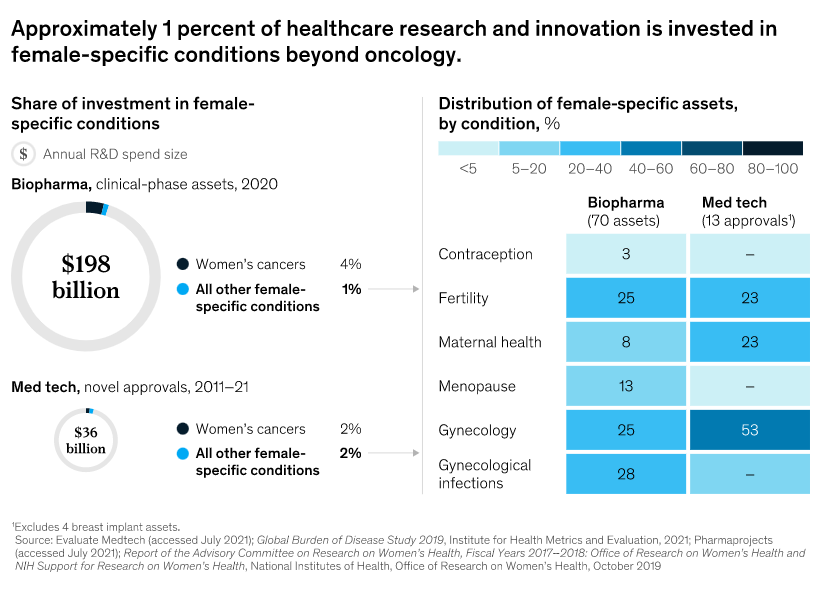
There are significant opportunities for healthcare providers to consider reallocating resources to female conditions, including the following:
Maternal health: More than 800 women die globally every day from pregnancy- and childbirth-related causes, including hemorrhages and infections.16 The tragedies are not confined to emerging economies; even before the outbreak of COVID-19, the maternal mortality rate in the United States doubled between 2002 and 2018, with Black women disproportionately affected.17
Endometriosis: One in ten women of reproductive age is estimated to have endometriosis (growth of endometrial tissue outside of the uterus), which can cause debilitating pelvic pain and infertility. The underlying pathophysiology is poorly understood, diagnosis takes ten years on average, and there is currently no cure.18
Menopause: Women spend more than a third of their lives in peri- or post-menopause, and trends indicate that 1.2 billion women globally will be in these life stages by 2030.19 The vast majority of women find that menopausal symptoms such as hot flashes, night sweats, and sleep disturbances interfere with their lives, yet only a quarter obtain treatment.20 The economic impact is significant, with one study estimating nearly $1,400 in health costs and $770 in lost productivity per person per year for untreated hot flashes alone.21
There is great potential to begin addressing these conditions in new ways. A suite of scientific advances can now be harnessed in women’s health. Recent advances in genomics, tissue engineering, and cell and gene therapy are ushering in a new wave of healthcare innovations that can be applied to underserved female-specific conditions. For example, researchers are studying transcriptomics (the study of all RNA molecules in a cell) for treating otherwise elusive conditions such as preeclampsia or preterm birth. Others are now using tissue engineering to create uterine organoids in order to push the knowledge frontier on endometriosis. The potential is vast to redefine a host of conditions, including endometriosis, preeclampsia, and unexplained infertility, and to achieve advances to the degree that researchers are already achieving with oncology and immunology. Investors, researchers, and companies alike have an opportunity to participate in this rising wave of innovation and to deliver a new era in women’s health.
Arizona Health Care Cost Containment System (AHCCCS) is Arizona's Medicaid agency that offers health care programs to serve Arizona residents. Individuals must meet certain income and other requirements to obtain services.
The Arizona Center for Rural Health (AzCRH) core mission is to improve the health and wellness of Arizona’s rural and underserved populations. AzCRH houses programs including:
State Office of Rural Health (AzSORH)
Rural Hospital Flexibility Program (AzFlex)
ADHS-CDC COVID Disparities Initiative (CDC-ADHS-AzCRH ISA)
Small Rural Hospital Improvement Program (AzSHIP)
Arizona First Responders Initiative (FR-CARA)
Workforce Data & Analysis (CRHWorks)
MEZCOPH Rural Health Professions Program (RHPP)
Students Helping Arizona Register Everyone (SHARE) and Health Insurance Help
Arizona Rural Recruitment and Retention Network (Az3RNet)
Arizona Department of Health Services ADHS-AzCRH Interagency Service Agreements:
The Office of Minority Health is dedicated to improving the health of racial and ethnic minority populations through the development of health policies and programs that will help eliminate health disparities.